Revolutionizing Joint Health: The Role of Arthroplasty
Introduction
Arthroplasty, commonly known as joint replacement surgery, is a surgical procedure designed to restore the function of a joint by replacing damaged or diseased joint surfaces with artificial components. This procedure is most frequently performed on joints such as the hip, knee, shoulder, and elbow, where severe arthritis or injury has led to significant pain, stiffness, and impaired movement. Arthroplasty has revolutionized the treatment of joint disorders, providing millions of people worldwide with relief from chronic pain and improved quality of life. This comprehensive article explores the concept of arthroplasty, including its history, indications, types, surgical techniques, postoperative care, outcomes, and future advancements.
History of Arthroplasty
The history of arthroplasty dates back to the early 20th century, with significant advancements occurring over the decades. The development of modern joint replacement surgery can be traced through several key milestones:
- Early Attempts: In the early 1900s, surgeons experimented with various materials, including ivory and glass, to replace damaged joint surfaces. However, these early attempts were largely unsuccessful due to issues with infection and material durability.
- Introduction of Metal Implants: In the 1940s and 1950s, the use of metal implants, such as stainless steel and cobalt-chromium alloys, marked a significant advancement. These materials were more durable and less prone to infection, leading to improved outcomes for patients.
- Sir John Charnley’s Contributions: In the 1960s, British orthopedic surgeon Sir John Charnley developed the concept of low-friction arthroplasty. He introduced the use of high-density polyethylene for the acetabular component (socket) and a metal femoral component (ball) in hip replacements. This combination significantly reduced wear and friction, leading to longer-lasting implants.
- Advancements in Materials and Techniques: Over the subsequent decades, advancements in materials science and surgical techniques further improved the outcomes of arthroplasty. The development of biocompatible materials, such as titanium and advanced ceramics, along with refined surgical approaches, has contributed to the success of modern joint replacement surgery.
Indications for Arthroplasty
Arthroplasty is primarily indicated for individuals suffering from severe joint pain and dysfunction that significantly affects their quality of life. Common indications include:
- Osteoarthritis: Osteoarthritis is the most common indication for arthroplasty. This degenerative joint disease leads to the breakdown of cartilage, causing pain, stiffness, and reduced joint mobility.
- Rheumatoid Arthritis: Rheumatoid arthritis is an autoimmune condition that causes inflammation of the joint lining, leading to pain, swelling, and joint damage. When conservative treatments fail, arthroplasty may be recommended.
- Post-Traumatic Arthritis: Joint injuries, such as fractures or ligament tears, can lead to post-traumatic arthritis, where the joint surfaces become damaged over time. Arthroplasty can help restore function and relieve pain in these cases.
- Avascular Necrosis: Avascular necrosis occurs when the blood supply to the bone is disrupted, leading to bone death and joint collapse. Arthroplasty may be necessary to replace the damaged joint surfaces.
- Congenital Deformities: Some individuals are born with joint deformities that affect function and cause pain. Arthroplasty can help correct these deformities and improve joint function.
- Failed Previous Joint Surgery: In some cases, previous joint surgeries, such as osteotomies or arthroscopic procedures, may fail to provide long-term relief. Arthroplasty can be considered as a salvage procedure.
Types of Arthroplasty
There are several types of arthroplasty, each designed to address specific joint conditions and patient needs. The most common types include:
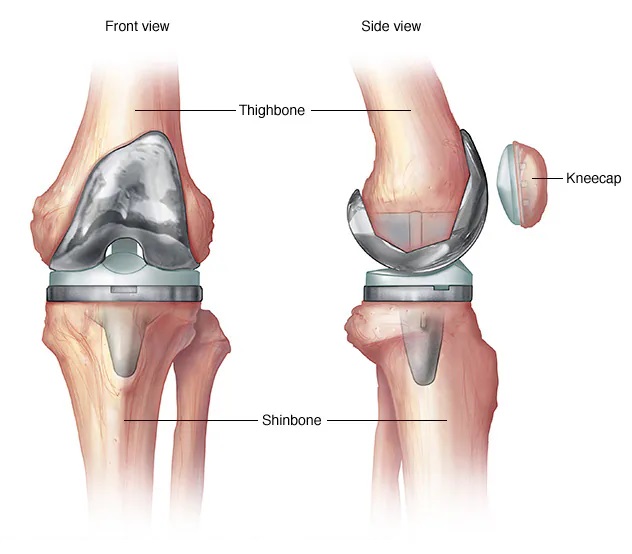
- Total Joint Arthroplasty (TJA): Total joint arthroplasty involves replacing both the damaged joint surfaces with artificial components. This is the most common type of arthroplasty and is frequently performed on the hip, knee, and shoulder joints.
- Partial Joint Arthroplasty: Partial joint arthroplasty, also known as hemiarthroplasty, involves replacing only one part of the joint. For example, in hip hemiarthroplasty, only the femoral head is replaced, while the acetabulum is left intact.
- Resurfacing Arthroplasty: Resurfacing arthroplasty involves replacing only the damaged surface of the joint while preserving as much of the natural bone as possible. This technique is often used in younger patients with early-stage joint disease.
- Revision Arthroplasty: Revision arthroplasty is performed when a previous joint replacement fails or wears out. It involves removing the old implant and replacing it with a new one.
Surgical Techniques in Arthroplasty
The surgical techniques used in arthroplasty have evolved significantly over the years, leading to improved outcomes and reduced complications. The key steps in a typical arthroplasty procedure include:
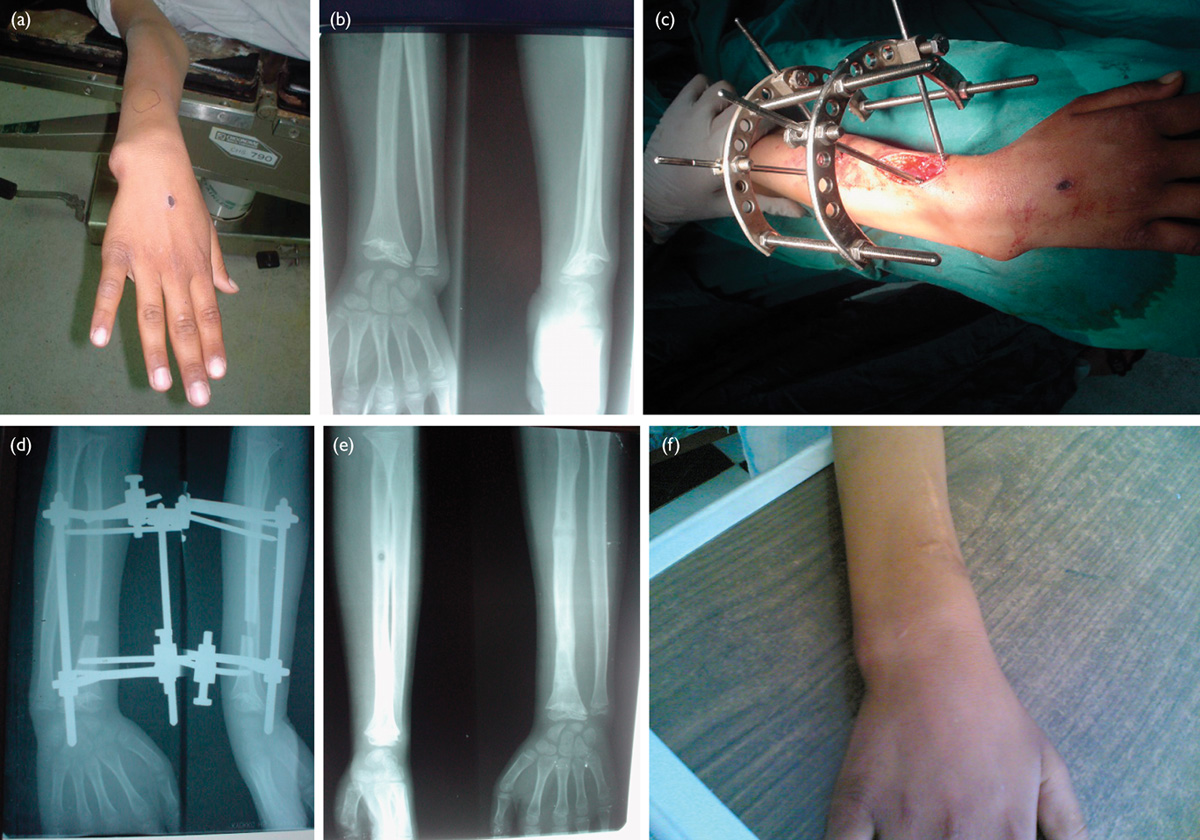
- Preoperative Planning: Preoperative planning involves a thorough assessment of the patient’s medical history, physical examination, and imaging studies, such as X-rays and MRI scans. This information helps the surgeon determine the appropriate implant size and type.
- Anesthesia: Arthroplasty is usually performed under general anesthesia or regional anesthesia, such as spinal or epidural anesthesia, depending on the patient’s condition and the surgeon’s preference.
- Incision and Exposure: The surgeon makes an incision over the joint to gain access to the damaged joint surfaces. The approach may vary depending on the joint being replaced.
- Bone Preparation: The damaged joint surfaces are removed, and the underlying bone is prepared to receive the artificial components. This involves shaping the bone to ensure a precise fit for the implant.
- Implant Placement: The artificial components, made of metal, plastic, or ceramic, are carefully placed and secured to the prepared bone surfaces. The components are designed to replicate the natural joint’s function and allow for smooth movement.
- Closure and Recovery: After the implants are in place, the surgical site is closed with sutures or staples, and a sterile dressing is applied. The patient is then taken to the recovery room for postoperative monitoring.
Postoperative Care and Rehabilitation
Postoperative care and rehabilitation are critical to the success of arthroplasty. The goals are to manage pain, prevent complications, and restore joint function. Key aspects of postoperative care include:
- Pain Management: Pain management is essential in the immediate postoperative period. A combination of medications, including opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), and local anesthetics, may be used to control pain.
- Wound Care: Proper wound care is essential to prevent infection. The surgical site should be kept clean and dry, and any signs of infection, such as redness, swelling, or drainage, should be promptly reported to the healthcare provider.
- Physical Therapy: Physical therapy is a crucial component of postoperative rehabilitation. Early mobilization and exercises help improve joint function, strength, and range of motion. Physical therapists work closely with patients to develop personalized rehabilitation programs.
- Assistive Devices: Assistive devices, such as crutches, walkers, or canes, may be used to aid mobility and reduce stress on the operated joint during the initial recovery period.
- Follow-up Appointments: Regular follow-up appointments with the surgeon are essential to monitor the healing process, assess joint function, and detect any potential complications.
Outcomes and Complications
Arthroplasty has a high success rate, with most patients experiencing significant pain relief and improved joint function. However, as with any surgical procedure, there are potential complications, including:
- Infection: Infection is a serious complication that can occur in the immediate postoperative period or years after surgery. Prompt treatment with antibiotics and, in severe cases, surgical intervention may be required.
- Implant Loosening: Over time, the artificial components may become loose, leading to pain and reduced joint function. Revision surgery may be necessary to address this issue.
- Dislocation: Dislocation of the artificial joint can occur, particularly in hip replacements. Proper surgical technique and patient education on movement restrictions can help prevent dislocations.
- Blood Clots: Blood clots, such as deep vein thrombosis (DVT) or pulmonary embolism (PE), are potential complications following arthroplasty. Blood-thinning medications and early mobilization can help reduce the risk.
- Nerve or Blood Vessel Injury: Damage to nerves or blood vessels near the surgical site is a rare but possible complication. Careful surgical technique and thorough preoperative planning can minimize this risk.
Advances in Arthroplasty
Advances in medical technology and research continue to improve the outcomes and safety of arthroplasty. Some notable advancements include:
- Minimally Invasive Techniques: Minimally invasive surgical techniques involve smaller incisions and less tissue disruption, leading to faster recovery times and reduced postoperative pain.
- Computer-Assisted Surgery: Computer-assisted surgery and robotic-assisted surgery provide enhanced precision and accuracy in implant placement, leading to improved joint alignment and function.
- Improved Implant Materials: The development of advanced implant materials, such as highly cross-linked polyethylene and ceramic-on-ceramic bearings, has reduced wear and increased the longevity of joint replacements.
- Biologic Augmentation: Biologic augmentation involves the use of growth factors, stem cells, and other biological agents to enhance tissue healing and integration with the artificial components.
- Personalized Implants: Advances in 3D printing technology have enabled the production of personalized implants tailored to the patient’s unique anatomy, improving fit and function.
Future Directions in Arthroplasty
The future of arthroplasty holds promise for even greater advancements in patient care and outcomes. Some exciting areas of research and development include:
- Regenerative Medicine: Regenerative medicine aims to develop techniques to regenerate damaged joint tissues using stem cells, growth factors, and tissue engineering. This approach has the potential to provide long-term solutions for joint disorders without the need for artificial implants.
- Smart Implants: Smart implants equipped with sensors and wireless technology can provide real-time data on joint function, load distribution, and wear patterns. This information can be used to monitor implant performance and detect issues early.
- Enhanced Rehabilitation Techniques: Advances in rehabilitation techniques, such as virtual reality (VR) and tele-rehabilitation, offer innovative ways to engage patients in their recovery process and improve outcomes.
- Prevention Strategies: Research into the prevention of joint diseases, such as osteoarthritis, through lifestyle modifications, early interventions, and genetic therapies holds promise for reducing the need for arthroplasty in the future.
Conclusion
Arthroplasty is a transformative surgical procedure that has significantly improved the quality of life for individuals suffering from severe joint pain and dysfunction. With a rich history of advancements and ongoing innovations in surgical techniques, implant materials, and rehabilitation methods, arthroplasty continues to evolve, offering better outcomes and increased longevity of joint replacements. As research in regenerative medicine, smart implants, and personalized care advances, the future of arthroplasty holds great promise for even more effective and less invasive treatments for joint disorders.



Leave a Reply